Please Follow us on Gab, Minds, Telegram, Rumble, Gettr, Truth Social, Twitter
In the harrowing years of World War II, the Nazi regime, under Adolf Hitler, pursued an insidious policy aimed at creating the so-called "Aryan" master race. This ideology led to the systematic persecution and extermination of groups deemed "inferior" or "undesirable," including Jews, Romani people, disabled individuals, and others. The Holocaust, the most infamous example of this genocidal policy, saw six million Jews systematically murdered. Programs like the T4 Euthanasia Program targeted individuals with physical and mental disabilities, resulting in the murder of tens of thousands. Elderly individuals, seen as unproductive or burdensome, were also targeted.
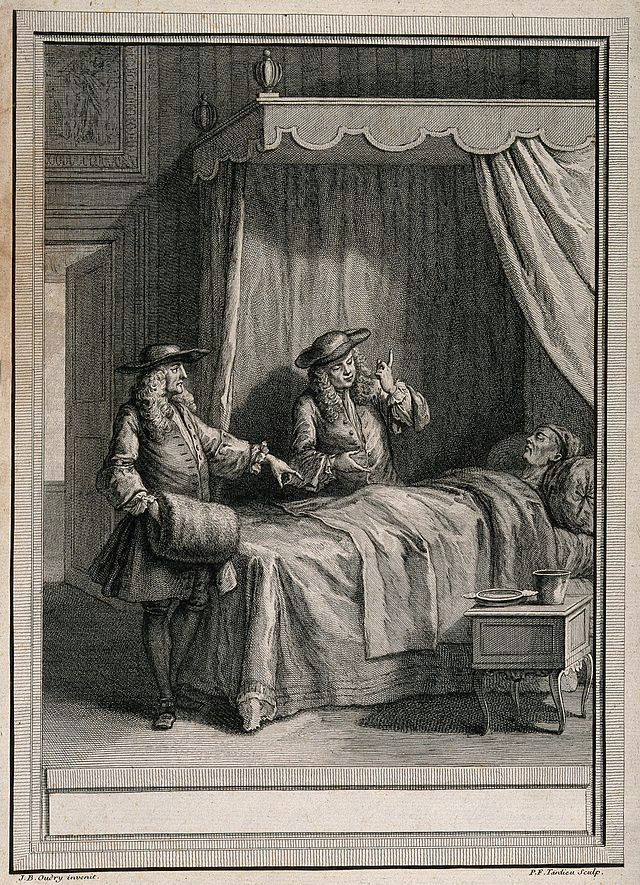
Fast forward to today, and the language of medical care—terms like "Do Not Resuscitate (DNR)," "intubate," "palliative care," and "quality of life"—shapes critical end-of-life decisions. These terms are designed to respect patient autonomy and ensure compassionate care, but they also raise complex ethical questions.
Modern Medical Terms and Their Implications
Personal Experience and Ethical Considerations
Reflecting on my personal experiences underscores the complexities inherent in these terms. In 2003, my father was intubated for 14 days. When he went to the hospital, his mind was clear. Upon discharge, they claimed he had two weeks to live and had developed dementia. Remarkably, he lived for four more years, and within two weeks, it was evident he did not have dementia. This experience raised questions about the accuracy of medical assessments and the profound impact of critical care interventions.
Recently, I faced a similar situation with a loved one who is mentally challenged. He was critically ill with sepsis and unable to eat. The decision not to resuscitate or intubate him was straightforward, but withholding food felt like a death sentence. Thankfully, he responded well to antibiotics and began to recover. This mirrored my father's experience, where an initial grim prognosis proved incorrect.
Quality of Life: Who Decides?
Determining quality of life is a deeply ethical question. Ideally, this should involve the patient's wishes, medical professionals' assessments, and input from family members. However, the balance of these perspectives can be challenging, and subjective judgments can influence decisions. This concern is not unfounded; it echoes historical atrocities where subjective judgments led to the devaluation of human lives.
Palliative Care: Ethical Boundaries
Palliative care aims to alleviate suffering and improve the quality of life. Yet, decisions about nutrition and hydration are ethically complex. In cases where a patient cannot eat due to illness, the use of artificial nutrition must be carefully considered. The benefits and burdens should be weighed, always prioritizing the patient's comfort and dignity.
Avoiding Historical Mistakes
My experiences and reflections emphasize the need for compassionate and ethical care in medicine. It is crucial that medical decisions are made with respect for individual dignity and a focus on the well-being of the patient. We must remain vigilant to ensure that our approach to medical care does not echo the inhumane practices of the past.
In conclusion, as we navigate the complexities of modern medical care, let us commit to compassionate, ethical, and patient-centered practices. Only through such an approach can we honor the dignity and value of every individual, ensuring that history's darkest chapters are never repeated.